Request Free Demo:
Mobile#: +966547315697
Email: sales@bilytica.com
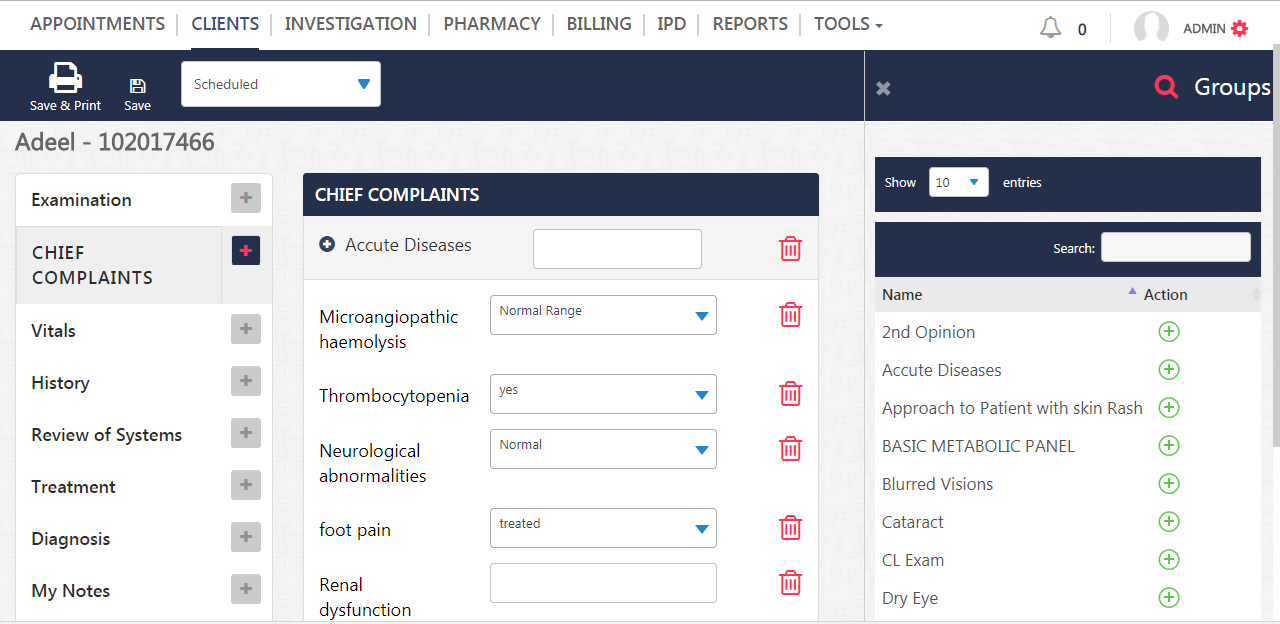
Cloudpital hospital management software further immersed ourselves in the auditory pitfalls of an E & M medical audit, the second part of our four-part series focused on the importance of a well-documented major complaint and HPI, since it was a big stumbling block in suppliers trying to pass an audit. The auditor relies on the documentation of the problem that is presented to give the doctor the medical necessity support to advance with his documentation of a record.
As we move to the third part of our series, this week, an important pitfall in an audited record comes from the Electronic Medical Record (EMR) and not necessarily from the physician’s or provider’s attempt at documentation.
https://www.youtube.com/watch?v=17wxU-LZduM&t=7s
Specialty of EMR Software :
- Dentistry EMR
- Nephrology EMR
- Community Health EMR
- Hematology EMR
- Psychiatry EMR
- Psychiatry EMR
- Ophthalmology EMR
- Pain Management EMR
- Plastic Surgery EMR
- Internal Medicine EMR
- Physical Therapy EMR
- Dermatology EMR
- Pediatrics EMR
- ENT EMR
- Mental Health EMR
- Podiatry EMR
- Gynecology EMR
- Cardiology EMR
- Family Practice EMR
- Orthopedic Surgery EMR
- Neurology EMR
- Diabetology EMR
- Pulmonary EMR
- Gastroenterology EMR
- Urology EMR
Most electronic health record systems include software to help providers determine the appropriate CPT assessment and administration (E & M) codes for patient encounters. If used correctly, these tools do support accurate coding based on medical necessity and have been associated with generally higher levels of E & M coding. However, as I audit the practices of physicians using the EHR records / EMR, I find significant flaws in EHR software design, inadequate implementations and a general lack of user knowledge about how E & M coding systems work.
Recommend E & M codes:
The Office of the Inspector General (OIG) of the Cloudpital electronic medical record (EMR) software Health and Human Services. UU He has documented well his concerns about EMRs that “help” providers with coding and documentation decisions, but there has been little external evidence of how EMRs capture and use information to recommend E & M codes. All electronic medical record systems include features that support (at least partially) the precise E & M coding; but all have discrepancies that could cause incorrect coding. In most health care settings, the doctor is responsible for choosing the code, which puts the responsibility for incorrect coding only on the shoulders of the provider. To avoid denials, rejections, sanctions and even accusations of fraud, providers and coding professionals must understand how electronic health record software and their limitations are designed.
Services WE Offer:
-
Practice Management
- EMR
- EClinic
- Revenue Management
- Patient Referral Software
- Mobile Health
- Patient Portal
- Telemedicine EMR
- Appointment Management
- Registration and Inquiry
- Specialty EMR
-
Hospital
- Hospital Management
- EMR
- Laboratory Software
- In Patient ADT Management
- Radiology Machine Interfacing
- Pharmacy Software
- Duty Roster
- Nursing & Wards Management
- Pathology Lab Software
-
Enterprise
- Enterprise HR & Payroll
- Enterprise Billing
- Financial Accounting
- PACS & Radiology ( RIMS)
- Operation Theatre Management
- Bed Census Software
- Casualty & Emergency
- Inventory & Warehouse
Automatically Identify Key Data Element:
A consistent trend I see is the inability of EMRs to automatically identify key data elements related to the complexity of medical decision making. This suggests to me that, in general, EMRs do not capture the key encounter information necessary to support accurate computer-assisted E & M coding. Providers often rely on EMRs to guide their documentation related to coding. eClinic Software inability of a system to document information related to E & M key in a structured format can lead to errors in the documentation and suggest lower E & M codes. Remember that an audit is, in effect, a scoring system.
